If I’m telling the truth, the new stimulator was just not working the same as the first one unfortunately. I was frustrated and had a few different adjustments, but it just was not taking care of the pain like the first one. We’ll call it the 80% experiment that would soon go wrong.
It was Monday of this week around lunchtime. My mom had come by work (which I had just returned to) for us to go and have lunch together. That’s when I noticed that my implanted battery felt like someone had reached inside and twisted it around. It was burning and it soon hurt like hell. From then on the pain grew worse and by the time I got in the car to drive home I was in screaming pain. The pain had spread up my spine as well.
An after hours phone call from Dr. Sayed led to a first thing visit the next morning.
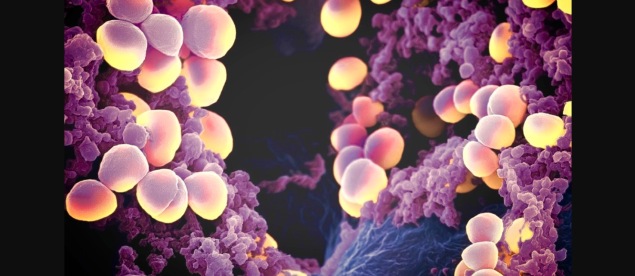
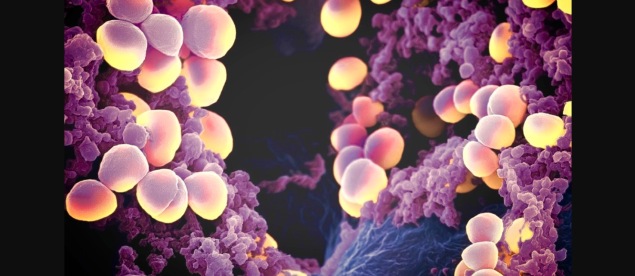
Overnight, the device, leads and incisions were obviously infected. A red, raised rash with a fever had formed. I was also running a fever at this point.
Dr. Sayed took one look and said I was being admitted through the emergency room. And that the device would likely need to be removed today.
I was in disbelief, as was my fiancée, Brian. How could the surgical site become infected nearly five weeks after the surgery?
The next thing I knew, I was prepped for surgery and in the holding room. Now, this is when 50 people come in and all talk quickly and loudly. Ok, not 50, but for the size of the room it was too much. I started to panic. The anesthetist immediately injects versed to calm me down. And then I’m off to surgery.
It’s amazing how quickly everything happened when you consider how long you wait for your surgery to even be scheduled. But that’s another story.
It turns out I had a staph infection. Luckily, it was MSSA. The device was removed and the entire area cleaned out.
I spent the next 3 days in the hospital being pimped full of antibiotics and pain meds. I ordered whatever I wanted to eat from the glorious hospital menu. Because why not at this point?
So, three surgeries later and I’m back at square one. I do want to be clear that the doctor and Herb informed me that I was the first to break a device and first to have an infection. So this is not the norm.
But now I am waiting for the inevitable: the old pain to come slithering back (which has already started) and wondering what on earth to do next. Dr. Sayed said we could redo the surgery in a couple months, but I feel like my body just does not want that foreign object.
I wish that the old pain would just be minimal and I could find a different way to address it. Only time will tell.
So yeah, I’m discouraged. Anyone would be. Thankfully I have a pretty good support system of family, Brian, and friends.
 I honestly never thought I’d be able to do any of these things again – so yes, there is hope! Take good care of yourself!
I honestly never thought I’d be able to do any of these things again – so yes, there is hope! Take good care of yourself!